As the nation navigates the complexities of mental health care, the attention surrounding Attention Deficit Hyperactivity Disorder (ADHD) has intensified, prompting a pivotal examination of the policies that shape its management. In the wake of the Trump administration, which has often been characterized by its distinctive approach to health care, there arises a critical question: what does the future hold for ADHD care under officials drawn from conservative ideologies? This article seeks to explore the potential shifts in ADHD treatment and support—an intersection of politics, personal experience, and medical practice—while considering the implications these policies may have for individuals and families battling this prevalent condition. With perspectives ranging from regulatory changes to funding reallocation, we delve into the evolving landscape of ADHD care and its alignment with broader conservative health strategies, unearthing the potential consequences for millions of Americans living with ADHD.
Table of Contents
- Reevaluating Treatment Paradigms for ADHD: The Impact of Political Leadership
- Integrating Behavioral Interventions: Balancing Medication and Therapy in ADHD Care
- Access and Affordability: Navigating Policy Changes for ADHD Services
- Empowering Families: Advocacy and Resources for Future ADHD Care Improvements
- Q&A
- In Retrospect

Reevaluating Treatment Paradigms for ADHD: The Impact of Political Leadership
As the landscape of ADHD care shifts under the influence of new political leadership, the approaches to diagnosis and treatment are being scrutinized from multiple angles. With a focus on evidence-based practices, conservative policies may prioritize streamlined protocols that emphasize cost-effectiveness and accessibility. This transformation could lead to a heightened emphasis on non-pharmacological interventions as principal tools for managing symptoms. Increased funding for public education initiatives and support services may emerge as an alternative to medication, as stakeholders debate the broader societal implications of ADHD treatment.
Furthermore, the leadership may advocate for a more family-centric treatment model. This paradigm shift might involve empowering parents and caregivers through enhanced training programs and resources, offering a collaborative approach that includes behavioral therapies alongside or in place of traditional medical interventions. The potential establishment of community support networks could play a pivotal role in facilitating peer support and information exchange among families navigating ADHD, fostering resilience and understanding. Here is a brief illustration of how these elements might be prioritized:
| Focus Areas | Potential Initiatives |
|---|---|
| Public Awareness | Education campaigns on ADHD |
| Non-Pharmacological Treatments | Promote cognitive behavioral therapy |
| Family Involvement | Workshops for parents and caregivers |
| Community Resources | Development of local support groups |
Integrating Behavioral Interventions: Balancing Medication and Therapy in ADHD Care
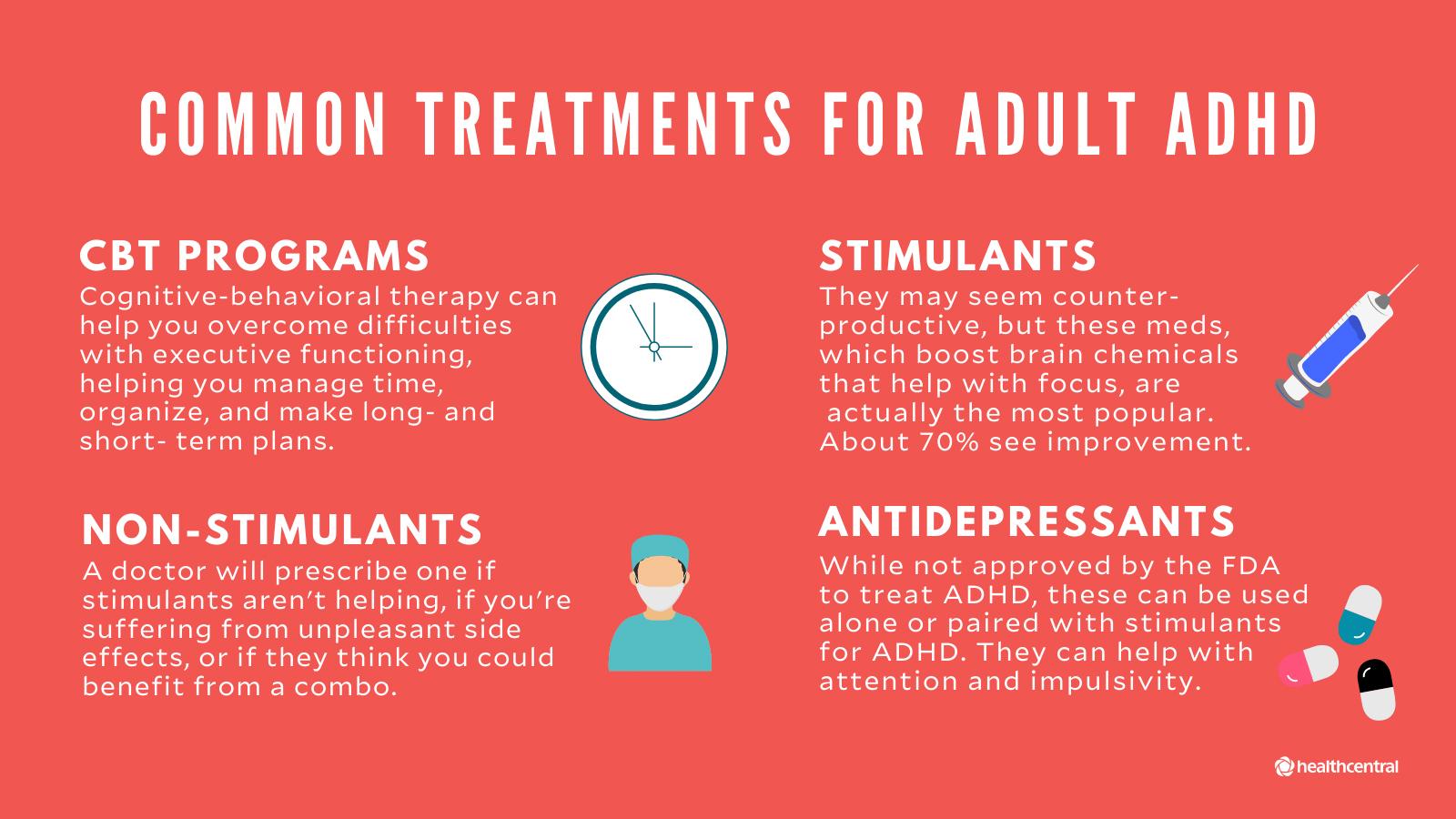
As the conversation surrounding ADHD treatment evolves, the integration of behavioral interventions has become increasingly vital. With a more conservative approach to healthcare potentially on the horizon, it is essential to emphasize a balanced strategy that includes both medication and therapy. While medications like stimulants can effectively manage symptoms, they do not address the underlying behavioral issues that often accompany ADHD. Therefore, therapists and healthcare providers must develop tailored treatment plans that incorporate evidence-based behavioral strategies along with pharmaceutical support. This multidimensional approach can lead to more sustainable long-term outcomes for individuals living with ADHD.
Identifying effective behavioral interventions is paramount for achieving holistic care. By focusing on a combination of techniques, such as cognitive-behavioral therapy, parent training, and social skills development, providers can enhance the quality of life for ADHD patients. A survey of various approaches might reveal the following considerations:
| Intervention Type | Key Benefits |
|---|---|
| Parent Training | Improves parent-child interactions and behavior management. |
| Cognitive-Behavioral Therapy | Helps in developing coping strategies and self-regulation skills. |
| Social Skills Training | Enhances peer interactions and reduces social isolation. |
This combination fosters a collaborative atmosphere between clinicians, patients, and families, ultimately reinforcing the value of therapy in conjunction with medication. As policymakers set the stage for future ADHD care strategies, prioritizing integrated models will be crucial in ensuring effective, comprehensive support for those affected by this disorder.
The ongoing policy shifts under the Trump administration have stirred debate among advocates for ADHD services regarding their accessibility and affordability. As new regulations emerge, families relying on these essential healthcare services face uncertainties about their future. To navigate this landscape, stakeholders must consider various factors impacting the provision of ADHD care:
- Insurance Coverage: Changes in regulations may lead to differences in what is covered for ADHD treatments, influencing out-of-pocket expenses for families.
- Availability of Resources: Potential cuts to funding for mental health resources could limit access to critical ADHD services.
- Provider Networks: The composition of healthcare provider networks might shift, affecting the availability of specialists trained to manage ADHD.
Furthermore, the implications of shifting policies could reshape the teetering balance of affordability in ADHD care. Families may have to weigh their options between public services and private treatment plans, potentially leading to increased disparities in care quality. To illustrate the evolving landscape, consider the following table that outlines potential impacts of the policy changes:
| Impact Area | Potential Outcome |
|---|---|
| Insurance Reforms | Increased out-of-pocket costs for families |
| Funding Cuts | Reduced access to community support programs |
| Provider Availability | Longer wait times for appointments with ADHD specialists |
Empowering Families: Advocacy and Resources for Future ADHD Care Improvements
In a landscape where ADHD care is constantly evolving, families play an essential role in shaping the future of advocacy and resource allocation. As health policies shift, particularly under a more conservative approach, families must be equipped with the tools and support systems necessary to navigate these changes effectively. This calls for a collaborative effort to ensure that the voices of those affected by ADHD are heard clearly in policy-making discussions. Key areas of focus should include:
- Access to Resources: Families need comprehensive information on available therapies, medications, and educational adjustments.
- Community Support: Local parent-led networks should be strengthened to provide real-time assistance and shared experiences.
- Policy Engagement: Training families to advocate for their rights and communicate with policymakers ensures their needs are prioritized.
To visualize the impact of upcoming policy changes on ADHD care, families must track specific resources and their corresponding accessibility as proposed by health officials. The following table outlines potential areas of concern and focus:
| Resource Area | Current Accessibility | Proposed Changes |
|---|---|---|
| Medication Availability | Moderate | Increased regulation |
| Therapeutic Services | Limited | Expansion of local services |
| School Resources | Variable | Standardized approaches |
Empowering families will involve not only understanding these dynamics but also actively participating in the dialogue surrounding ADHD care. By advocating for resources that foster better outcomes, families can help shape a more inclusive environment that addresses the evolving needs of children with ADHD.
Q&A
Q&A: The Future of ADHD Care Under Trump’s Health Officials
Q1: What are the key changes anticipated in ADHD care under the Trump administration’s health officials?
A1: Under the Trump administration, there may be a noticeable shift towards conservative policies that prioritize reduced government intervention in healthcare. This could lead to changes in funding for public health programs, potentially impacting ADHD care access and the overall approach to mental health services.
Q2: How might these conservative policies affect access to ADHD diagnosis and treatment?
A2: Conservative policies often advocate for reduced regulation, which might streamline the diagnosis process but could also lead to fewer resources for comprehensive care. Access to ADHD diagnosis and treatment may become more contingent on private insurance coverage, impacting lower-income families who rely on public health resources.
Q3: What implications could arise from a shift in funding priorities for mental health services?
A3: If funding is reallocated away from mental health services, we might see longer waiting times for ADHD assessments and treatments. This could exacerbate existing disparities, leaving underserved populations with limited access to effective care or support systems.
Q4: How do current trends in ADHD research and treatment align with these potential policy shifts?
A4: Current ADHD research emphasizes the need for multi-faceted treatment approaches, including both medication and behavioral therapies. While conservative policies may focus on cost-cutting measures, there is a risk that this holistic approach could be overshadowed by a more narrow focus on medication management, potentially stigmatizing individuals who seek comprehensive care.
Q5: What role will education and advocacy play in shaping the future of ADHD care?
A5: As the landscape of ADHD care evolves, education and advocacy will be crucial. Stakeholders, including parents, educators, and healthcare professionals, will need to actively participate in dialogue with policymakers to ensure that the voices of those affected by ADHD are heard and that appropriate resources remain available.
Q6: What can individuals do to stay informed and engaged about changes in ADHD care?
A6: Individuals can stay informed by following reputable sources for updates on policy changes, engaging with local advocacy groups, and participating in community forums. Sharing experiences and knowledge can also empower families affected by ADHD to advocate for their needs and contribute to ongoing discussions about care options.
Q7: In what ways can practitioners adapt to these shifting policies while maintaining quality care?
A7: Practitioners can adapt by seeking creative solutions, such as telehealth options, community partnerships, and emphasizing preventive care strategies. Staying abreast of policy changes and advocating for evidence-based practices will also be vital in maintaining quality care under evolving policy frameworks.
Q8: What important considerations should families keep in mind as they navigate future ADHD care?
A8: Families should remain proactive about understanding their rights regarding healthcare access and be prepared to advocate for their children’s needs. It’s also essential to remain informed about the availability of resources, whether through public programs or community services, as these could change significantly under new policies. — This Q&A format aims to unpack the complexities surrounding anticipated changes in ADHD care under the Trump administration, offering insight while maintaining a balanced tone.
In Retrospect
As we embark on this uncertain journey into the future of ADHD care under the stewardship of Trump’s health officials, it is crucial to recognize the multifaceted nature of policy formation and its profound impact on those affected by attention disorders. The potential shift toward conservative policies may reshape the landscape of treatment, access, and support for individuals living with ADHD. As families navigate this evolving terrain, staying informed and engaged will be paramount. The dialogue around mental health care must remain inclusive and responsive to the diverse needs of those it serves. Whether through advocacy, research, or personal narratives, collective voices can influence the direction of care in a way that prioritizes well-being and understanding over division. In essence, while the future may hold challenges, it also presents opportunities for collaboration and advocacy. As we look ahead, may we strive for a system that embodies empathy and innovation, ensuring that ADHD care remains a priority for all stakeholders involved. The conversation has only just begun.
Dr. Jonathon Preston is a respected mental health specialist dedicated to helping individuals overcome challenges. With advanced training in psychology and decades of experience in the mental health field.
