In the ever-evolving landscape of healthcare, few topics spark as much debate as the coverage of Attention Deficit Hyperactivity Disorder (ADHD). For millions of individuals and families, understanding the intricacies of ADHD treatment options can often feel like navigating a labyrinth of policies and procedures. Enter the Trump-Kennedy insights—a unique convergence of perspectives that sheds light on ADHD coverage in today’s complex health system. This article aims to unravel these insights, offering a thoughtful examination of how political frameworks and healthcare policies intersect to shape the experiences of those affected by ADHD. Whether you are a caregiver, advocate, or simply seeking clarity in a multifaceted issue, join us as we explore the pathways to understanding and enhancing ADHD care through the lens of these prominent healthcare ideologies.
Understanding the Landscape of ADHD Treatment Coverage
When navigating the intricacies of ADHD treatment coverage, it is crucial to recognize the diversity in policy options available. Each insurance plan can vary significantly in terms of what medications are covered, the range of therapy options, and the overall support provided for ADHD management. Patients and their families should consider the following key factors to ensure comprehensive coverage:
- Type of Treatment: Many plans offer different levels of support for medications, psychotherapy, behavioral therapies, and educational interventions.
- Co-pays and Deductibles: Understanding the financial commitments required for both routine visits and prescriptions can alleviate unexpected financial burdens.
- Provider Network: Make sure to verify if your preferred providers or treatment centers are covered under your policy to avoid out-of-network fees.
Furthermore, it’s important to stay informed about current legislative changes that may affect coverage options. Regularly reviewing the specific terms outlined in your health policy could reveal potential gaps or opportunities for improved care. An overview of standard ADHD treatment components often covered by different insurers can be beneficial:
| Treatment Type | Typically Covered | Notes |
|---|---|---|
| Medication | Yes | Often includes stimulants and non-stimulants. |
| Therapy | Varies | Behavioral therapy is commonly covered; others may need pre-authorization. |
| Support Services | Sometimes | Educational support may depend on specific school policy agreements. |
Key Legislative Changes Impacting ADHD Care Accessibility
The evolving landscape of legislation surrounding ADHD care has ushered in significant changes aimed at improving accessibility to necessary treatments and resources. Key reforms have focused on ensuring insurance coverage adequately addresses ADHD diagnosis and management. Some of the critical changes include:
- Expanded Definition of Coverage: New policies now recognize ADHD as a chronic condition, mandating that insurers provide comprehensive coverage for both medication and therapy.
- Telehealth Accessibility: The shift towards telehealth has been supported by legislation, allowing patients to receive care remotely, an essential feature for those living in underserved areas.
- Parity Laws: Strengthened parity laws ensure that mental health services are treated on par with physical health services, reducing discrimination against ADHD treatments.
In addition to these reforms, legislators have introduced initiatives specifically aimed at reducing barriers to care. By mandating that schools provide specific accommodations for students with ADHD, the legislative framework now supports not only healthcare access but also educational needs. The following table highlights crucial legislative measures impacting ADHD care:
| Legislative Measure | Impact |
|---|---|
| Insurance Reform | Increased coverage for ADHD medications and therapy |
| Telehealth Expansion | Improved access to remote consultations |
| School Accommodation Mandates | Enhanced support for students with ADHD in educational settings |
Best Practices for Advocating Your ADHD Coverage Needs
When it comes to advocating for your ADHD coverage, preparation is key. Start by thoroughly understanding your policy and benefits, including what specific ADHD treatments and services are covered. Create a list detailing your needs, such as medication, therapy, or coaching, and gather relevant documentation, including diagnosis letters from your healthcare provider. Being organized will empower you during discussions with your insurance company. Additionally, don’t hesitate to seek support; consider connecting with advocacy groups or professionals who specialize in ADHD coverage. They can provide valuable insights and assistance tailored to your situation.
In your conversations with insurers, clarity and confidence are crucial. Use clear, concise language to explain your ADHD-related needs, and always reference your coverage rights. Consider these strategies to enhance your advocacy approach:
- Document Everything: Keep a record of all communications, including dates and names of representatives.
- Be Persistent: If you encounter roadblocks, don’t give up; follow up regularly until you receive a resolution.
- Know the Law: Familiarize yourself with relevant health care laws that protect your rights regarding mental health coverage.
To further support your advocacy efforts, utilizing a visual aid can help illustrate your needs and demonstrate the necessity of specific treatments. Below is a simple table that outlines common ADHD treatments and their typical costs, which may be pivotal in discussions with your insurer.
| Treatment | Typical Cost | Notes |
|---|---|---|
| Medication | $30-$300/month | Varies by brand and insurance plan |
| Therapy Sessions | $100-$250/session | Depends on provider and frequency |
| Coaching | $50-$150/hour | Can be covered under some plans |
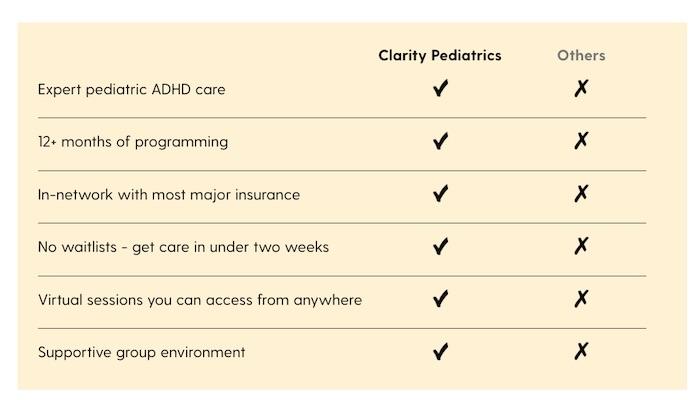
When navigating the intricate maze of insurance options for ADHD coverage, it’s crucial for families to first understand the various plans available. PPOs (Preferred Provider Organizations) offer flexibility in selecting healthcare providers, while HMOs (Health Maintenance Organizations) often provide lower premiums but require referrals for specialists. Additionally, families should look for plans that specifically cover ADHD-related services such as therapy, medication management, and educational assessments. A crucial element to consider is whether the plan includes in-network vs. out-of-network benefits, as this can impact out-of-pocket expenses significantly.
To assist families in evaluating these options, we can categorize coverage based on types of benefits available. Consider the following table as a comparison guide:
| Insurance Type | In-Network Benefits | Out-of-Network Coverage | Specialist Access |
|---|---|---|---|
| PPO | High coverage | Partial reimbursement | No referral needed |
| HMO | Lower premiums | No coverage | Referral required |
| EPO | High coverage | No coverage | No referral needed |
In addition to the type of plan, families should pay keen attention to specific coverage details for ADHD diagnoses. It’s also imperative to inquire about any limitations or exclusions tied to treatment types. This could include restrictions on the number of therapy sessions per year or specific medications that may not be covered. Armed with this knowledge, families can confidently advocate for their needs and make an informed decision that best supports their child’s well-being.
Q&A
Q&A: Navigating ADHD Coverage: Trump-Kennedy Health Care Insights Q1: What is the main focus of the article on ADHD coverage? A1: The article explores the complexities of ADHD coverage in the current healthcare landscape, particularly highlighting insights from the Trump-Kennedy health care policies. It examines how these policies impact access to treatment for individuals diagnosed with ADHD. Q2: How have recent political changes affected ADHD treatment options? A2: Recent political changes, notably under the Trump administration and the influence of Senator John F. Kennedy’s healthcare proposals, have led to shifts in funding and coverage priorities for mental health services, including those for ADHD. These changes can result in varying degrees of access to therapy and medication for those affected. Q3: Are there any specific policies mentioned that directly relate to ADHD coverage? A3: Yes, the article delves into specific provisions outlined in the Trump-Kennedy health care policies, such as increased funding for mental health services and initiatives aimed at improving insurance coverage for treatment options like behavioral therapy and medication management for ADHD. Q4: What challenges do families face in navigating ADHD coverage? A4: Families often encounter challenges such as insufficient insurance benefits, high out-of-pocket costs, and a lack of available specialists. The article outlines how these barriers can complicate the process of obtaining the necessary support and treatment for managing ADHD effectively. Q5: Does the article provide any practical tips for families dealing with ADHD? A5: Absolutely! The article offers practical tips, including how to effectively communicate with insurance providers, advocate for necessary services, and explore additional resources, such as community support programs, to ease the burden of ADHD management. Q6: How does the article address the importance of awareness and education surrounding ADHD? A6: The article emphasizes that increased awareness and education about ADHD are crucial for both families and healthcare providers. It encourages readers to understand the condition better and to advocate for comprehensive coverage, ensuring that individuals with ADHD receive the necessary care. Q7: What is the overarching message of the article? A7: The overarching message is that while navigating ADHD coverage can be challenging, it is essential for families to be informed and proactive. By understanding the implications of healthcare policies and utilizing available resources, individuals can better advocate for their needs and ensure access to effective treatment options.
To Wrap It Up
As we conclude our exploration of “Navigating ADHD Coverage: Trump-Kennedy Health Care Insights,” it’s clear that the landscape of healthcare for individuals with ADHD is both complex and evolving. The nuances of coverage—spanning policy changes, legislative influences, and individual circumstances—create a tapestry of challenges and opportunities. By analyzing the perspectives of key figures, we gain a deeper understanding of the pressing need for a comprehensive, compassionate approach to ADHD care. In a world where each diagnosis is as unique as the individual it represents, it is imperative that we advocate for clearer, more accessible paths to treatment and support. As we move forward, let us remain engaged and informed, continuously seeking to bridge the gaps in care and elevate the voices that often go unheard. The journey through ADHD coverage may be winding, but with insight and collaboration, we can pave the way to a more inclusive and understanding healthcare system for all. Thank you for joining us on this important discussion, and let’s continue the conversation about shaping a better future for those affected by ADHD.
Dr. Jonathon Preston is a respected mental health specialist dedicated to helping individuals overcome challenges. With advanced training in psychology and decades of experience in the mental health field.
